AI For Patient Eligibility and Benefits
AI with advanced workflow automation for challenging prior authorizations.

Offered with flexible fees models
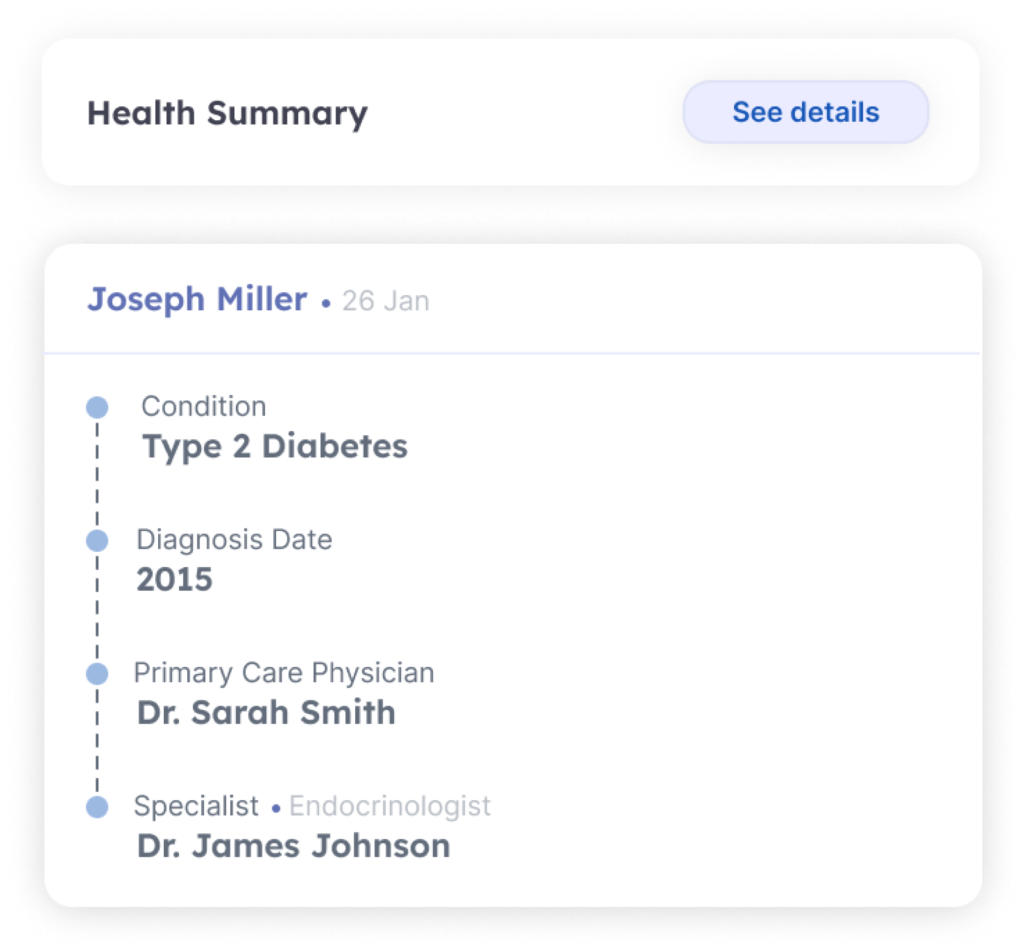
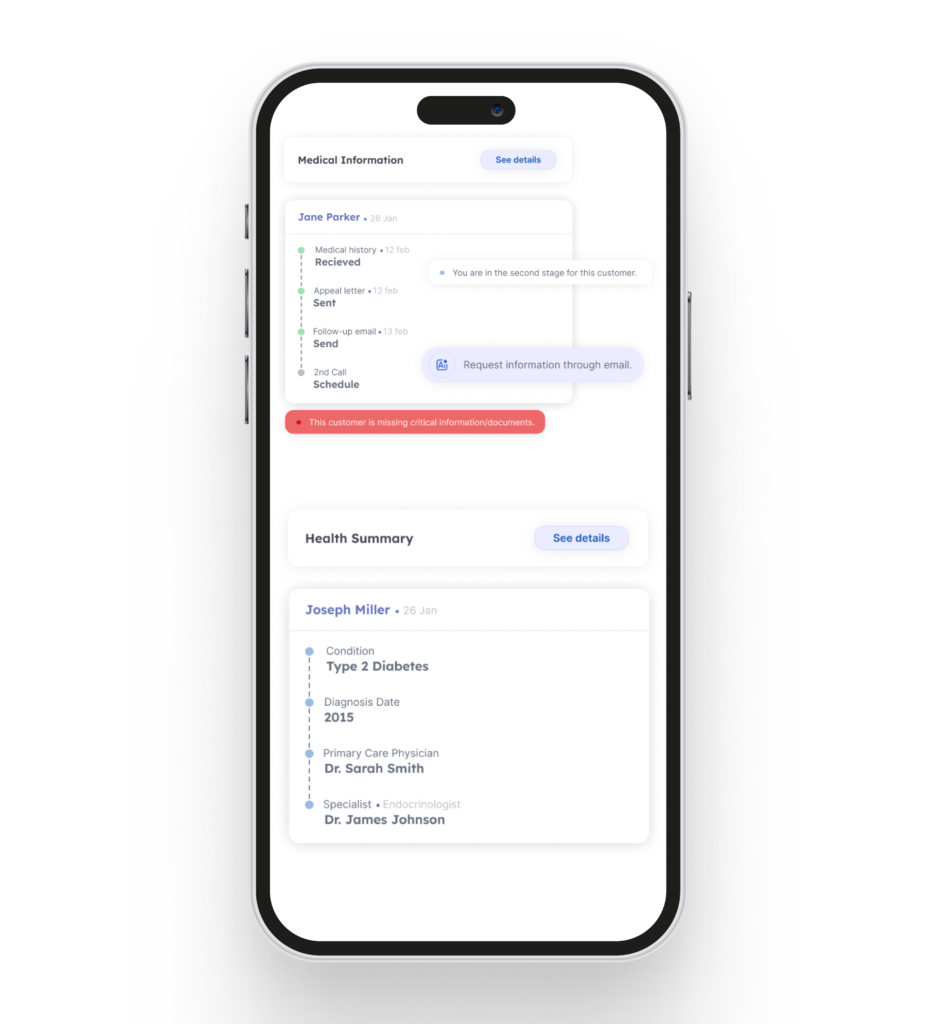
Benefit Investigations with AI
Manual benefit investigations are costly with delays in start of therapy.
Technology and Managed Services
- Faster Eligibility Verification: Quickly and accurately confirm patient eligibility, reducing wait times and accelerating the path to therapy initiation.
- Proactive Denials Management: Technology and humans teams to work the denial bucket for resolutions.
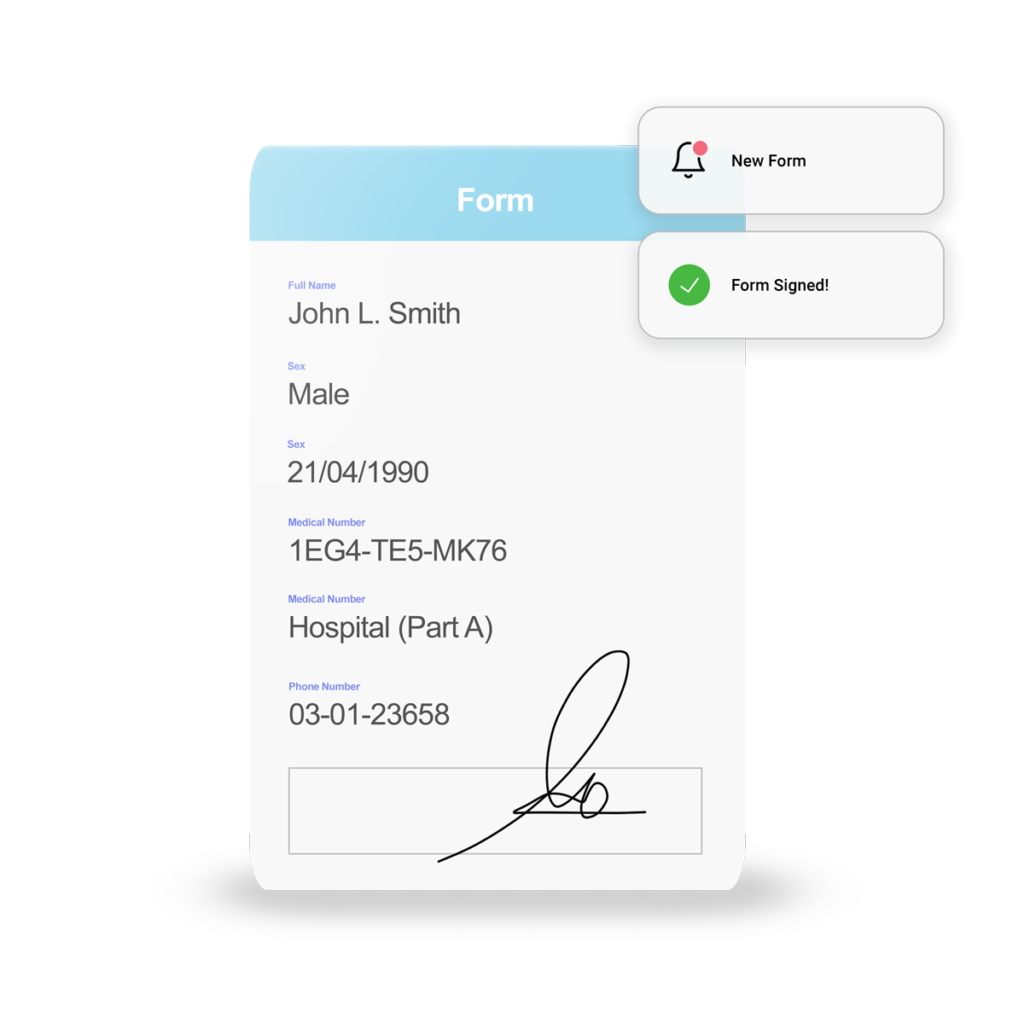
- Working Prior Authorization: Using technology to reduce staff work load to meet the requirements of payor for prior authorization process.
Patient Support Programs
Large language models for hyper personalized patient engagement.
Address therapy abandonment
Combination of intelligent and contextual contact with availability of care navigator.
Reduce Per Rx Dispense Hours
Protect the most valuable resource - Pharmacy staff time.
Pharmacy purpose-build automations